Ketamine Assisted Psychotherapy
A Novel & Rapid Experimental Treatment for Mood Disorders.
Ketamine Assisted Psychotherapy (KAP) - an experimental treatment that combines medically supervised use of Ketamine and psychotherapy - may rapidly alleviates depressive and suicidal symptoms within hours of treatment.
Depression is the leading cause of disability throughout the world! In the United States, depression affects one in six people sometime during their life, making them feel hopeless, unmotivated, or even suicidal. Therefore, antidepressants are big business, one of the most prescribed medications. Yet, all the current antidepressant drugs target the same kinds of brain chemistry!
Surprisingly, nearly half of depressed people do not experience significant benefits from these drugs. “Meta-analyses of antidepressant medications have reported only modest benefits over placebo treatment, and when unpublished trial data are included, the benefit falls below accepted criteria for clinical significance.” (Kirsch, I., Deacon, B., et al. (2008) Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration. PLoS Med, 5(2): e45).
_.jpeg)
Two of the worst side-effects of antidepressant drugs are: 1). A small but increased risk of suicide and
2). A high chance of provoking manic episodes in bipolar depressed patients, who are often incorrectly diagnosed. For all these reasons, better and more rapid treatments for depression are desperately needed.
Moreover, patients too often report undesirable side-effects like blurred vision, nervousness, headaches, sexual problems, or gastrointestinal (G.I.) pain.These medications affect the entire body, not such the brain.
Ketamine Assisted Psychotherapy
A research team at the National Institute of Mental Health, led by Dr. Carlos Zarate, found that a single dose of ketamine produced rapid antidepressant effects in depressed patients with bipolar disorder. After completing another controlled study, they reported: "Our finding that a single infusion of ketamine produces rapid antidepressant and anti-suicidal effects within one hour and that is fairly sustained is truly exciting," (Zarate, C., Nancy Brutsche, N., et. al. Replication of Ketamine's Antidepressant Efficacy in Bipolar Depression: A Randomized Controlled Add-On Trial. Biological Psychiatry, 2012; 71 (11): 939).
According to chief psychiatrist and ketamine researcher at Yale Medicine, “This is a game changer.” The drug works differently than those used previously, he notes, calling ketamine “the anti-medication” medication. “With most medications, like valium, the anti-anxiety effect you get only lasts when it is in your system. When the valium goes away, you can get rebound anxiety. When you take ketamine, it triggers reactions in your cortex that enable brain connections to regrow. It’s the reaction to ketamine, not the presence of ketamine in the body that constitutes its effects,” he says. (https://www.yalemedicine.org/stories/ketamine-depression/)
On March 5, 2019 the FDA approved a nasal spray derived from ketamine, esketamine, (which is far more expensive than cheaper forms of generic ketamine), that might be used at home for “treatment resistant” depression. Yet, the official recommendation is to continue with daily anti-depressant drug use – despite several previous trials of antidepressants not helping so-called “treatment resistant” patients. Moreover, the National Institute of Mental Health (NIMH) and the American Psychiatric Association (APA) have recommend the use of IV ketamine for psychiatric purposes. Yet, typically neither of these approaches fully integrate psychotherapy self-regulation and lifestyle skills that can further optimize the short-term window of opportunity provided by ketamine.
"It's the reaction to ketamine, not the presence of ketamine in the body that constitutes its effects."
Ketamine therapy has been hailed in Science magazine as the “biggest breakthrough in depression research in a half century” and may provided fast-acting relief to those with chronic, previously untreatable, forms of depression with suicidal thoughts. Ketamine is one of the safest anesthetic drugs, often used with children and animals. Ketamine doesn’t risk heart or respiratory failure, as many other anesthetics do, so an attending anesthesiologist doctor is not required. Still there is a turf war starting on whom will profit from this new treatment. Drug companies are lining up to profit from new medications that work upon yet untapped neurotransmitter systems. Anesthesiologist doctors appear eager to expand their range and to treat depressed patients. Psychiatrist trained in mental health care, see an opportunity to prescribe rapid-acting ketamine treatments, along with prescription medications. Yet, all the above falls within the standard pharmaceutical/medical treatment models of mental illness.
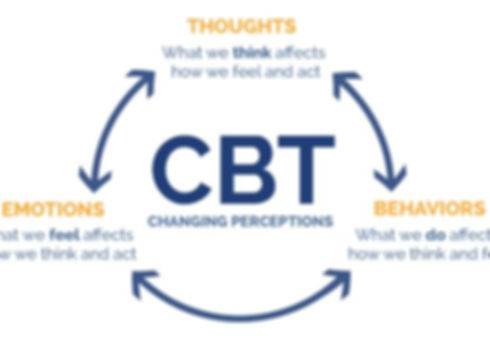
Ketamine does offer some surprisingly new ways to consider treatment. First ketamine represents the first class of legal psychedelic medications with an accepted psychiatric benefit. Known as a “dissociative anesthetic” when used in moderate doses; ketamine turns off sensory inputs and amplifies transpersonal (beyond ego) dream-like or mystical experiences. Unfortunately, ketamine can become addictive, if frequently misused, and even potentially dangerous when used beyond the safety of a clinic settings. Furthermore, treatment benefits captured during the transpersonal experiences might be as important as the shorter-term pharmaceutical effects. Increasingly researchers report that ketamine’s “dissociative” or transpersonal effects are essential for longer-term results. Ketamine treatments are especially promising when combined with cognitive-behavioral or transpersonal psychotherapies that help clients to transform their experiential states into positive changes of behaviors, beliefs and Self-acceptance. Ketamine Assisted Psychotherapy (KAP) is gaining acceptance among medical professionals at the KRIYA conferences (www.kriyainstitute.com), which psychologist Dr. Jeffrey Bruno and psychiatrist Dr. Max Burns, M.D. (www.maxburnsmd.com) attended. Together Dr. Burns and Dr. Bruno, after a careful initial screening, offer KAP to clients in a supervised clinic setting, for select those most likely to benefit.
Contact our office if you would like to learn more at Ketamine Assisted Psychotherapy (KAP).




